Abstract
T.N. was a 45-year-old African American female who presented with right breast swelling, pain, skin changes, and redness for 2 weeks (Figure 1). She was initially treated with antibiotics for presumed mastitis by her primary care physician. When she did not respond to the antibiotics, a mammogram was ordered; it was negative except for enlarged axillary lymph nodes. She eventually had a skin biopsy that showed invasive ductal carcinoma, poorly differentiated, with dermal lymphatic invasion; the tumor was hormone receptor negative and HER2/neu negative. Based on her clinical presentation and pathology, she was diagnosed with inflammatory breast cancer. It is interesting to note that initial staging did not reveal metastatic disease.
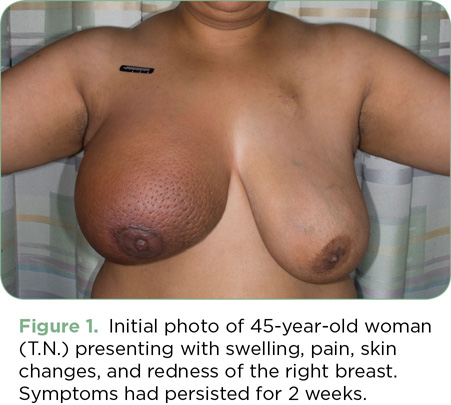
T.N. was treated with neoadjuvant taxane- and anthracycline-based chemotherapy, but only had a minimal response to the chemotherapy. She was deemed not to be a good surgical candidate at that time, and restaging scans revealed new metastatic disease to the bone. She then proceeded with palliative radiation therapy to the breast and nodal basin (with concurrent capecitabine [Xeloda]), which had to be halted due to significant skin desquamation. While recovering from radiation, she developed new chest wall lesions both inside and outside of the radiation field, contralateral breast involvement, bilateral lymphadenopathy, and bilateral pleural effusions (Figure 2). She subsequently received one cycle of carboplatin and gemcitabine, but she was admitted to the hospital with severe chest wall pain and increasing pleural effusions before receiving a second cycle. Eleven months from the time of diagnosis, T.N. died of her disease.