Abstract
Case Study
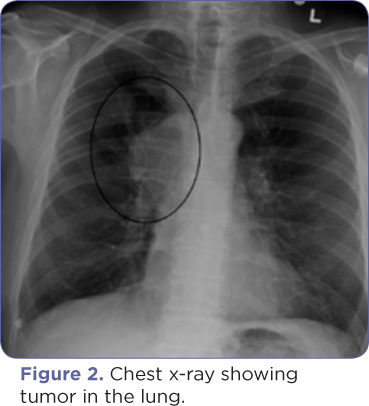
Mr. P. is a 67-year-old male who was originally seen by the pulmonologist after a chest x-ray revealed a right upper-lobe lung mass (Figure 2). Bronchoscopy revealed an extensive endobronchial tumor, and a biopsy was positive for small cell lung cancer. The patient was referred to the oncologist.3
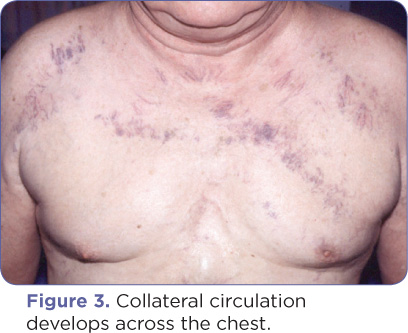
During the first oncology office visit, Mr. P. complained of increasing fatigue. He stated, "I become short of breath when I bend over. It lasts about 60 seconds, with some dizziness and head pain." Review of systems is positive for neck swelling noted in the morning, hoarseness of voice during the past week, purplish discoloration across his chest (Figure 3), thick vessels under his tongue, increased dyspnea on exertion, difficulty swallowing, and a dry cough lasting over a week. Pertinent physical findings are as follows: blood pressure 124/64, respirations 20, pulse 72 regular, temperature 97.8°; diffuse edema in the neck; dilated, engorged blood vessels on the chest and under the tongue; and edema in the left arm and hand.
Mr. P.'s current complaint is dyspnea, a sudden onset of a swollen neck, and a new diagnosis of small cell lung cancer. Because his symptoms are suggestive of superior vena cava syndrome (SVCS), which is potentially life threatening, he was immediately admitted to the hospital. A CT scan identified the source of the SVCS to be his malignancy. A CT angiogram also showed almost complete obstruction of the superior vena cava. The advanced practitioner’s admission orders included elevation of the head of the bed. In consultation with the collaborating physician, chemotherapy was immediately started. Mr. P. was in the hospital for 3 days as his symptoms responded quickly to the chemotherapy and he was able to breathe more easily. He was followed as an outpatient in the oncologist's office weekly for labwork and received chemotherapy every







