Abstract
Case Studies
Case 1
The first case we present is that of Mr. R., a 70-year-old Hispanic man with a diagnosis of unresectable World Health Organization grade II oligodendroglioma in bilateral frontal lobes. Although he did not have a high-grade malignancy, he received the same therapy as would a patient with a high-grade tumor. Mr. R. underwent standard radiotherapy and temozolomide (TMZ) chemotherapy. Bevacizumab (Avastin) was initiated at the time of tumor progression, which was 2 months after the completion of radiotherapy. At that time, Mr. R.’s visual acuity was 20/25 in both eyes without any corrective lenses. Pseudoprogression was ruled out with magnetic resonance (MR) spectroscopy and brain positron emission tomography (PET)/computed tomography (CT) before the start of bevacizumab treatment.
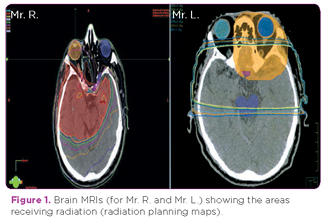
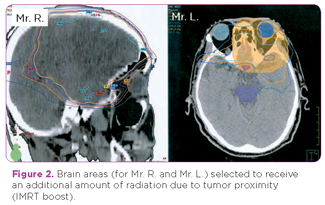
Mr. R. developed optic neuropathy 7 months after the initiation of bevacizumab therapy. His MRI remained stable throughout the bevacizumab therapy, with no tumor progression on either T1 contrast-enhanced or T2/FLAIR sequences. He lost the vision in his left eye first, followed by the vision in his right eye 2 months later. Neuro-ophthalmologic evaluation revealed no pallor in either optic nerve. The mean doses of radiation used were 50.6 Gy to the right optic nerve, 37.9 Gy to the left optic nerve, and 52.8 Gy to the optic chiasm. The tumor received 59.4 Gy in 33 fractions from both initial and intensity-modulated radiation therapy (IMRT) boost radiation treatments (see planning maps in Figures 1 and 2). Mr. R. developed bevacizumab-induced hypertension and was on amlodipine 5 mg daily. He had no evidence of tumor involvement with the optic nerves on MRI and no preexisting or new-onset diabetes mellitus.
After the onset of his blindness, Mr. R. developed depression, severe anxiety, and hallucinations related to having difficulty identifying the times of day. He was not on any medication that could have contributed to his anxiety or depression, such as a steroid or levetiracetam. Visual seizures were ruled out at the time. Mr. R. was also seeing vivid pictures. After a formal psychiatric evaluation, he was diagnosed with Charles Bonnet syndrome. Additionally, Mr. R. suffered several falls at home due to the loss of his vision. Mrs. R., the patient’s wife and primary caregiver, also developed anxiety as a result of taking care of her husband. Mr. R. eventually succumbed to his disease.
Case 2
The second case is that of Mr. L., an 82-year-old Asian man with glioblastoma multiforme in the left frontal lobe. Mr. L. received concomitant TMZ chemotherapy and radiotherapy. His tumor recurred 2 months after the completion of radiotherapy, and he was started on bevacizumab therapy. At that time, Mr. L.’s visual acuity was assessed as normal with corrective lenses to 20/40 in both eyes.
Mr. L. developed optic nerve neuropathy 14 months after the initiation of bevacizumab. He lost the vision in his right eye first, followed by that in his left eye 2 to 3 months later. Mr. L. met neither the McDonald nor the Revised Assessment in Neuro-Oncology (RANO) criteria for tumor progression. Neuro-ophthalmologic evaluation revealed right optic nerve pallor and atrophy and left optic nerve pallor. Mr. L.’s eyes were positive for retinal pigment epithelium changes as well as sclerotic vessels.
Mr. L. received 28.67 Gy to the right optic nerve, 32.7 Gy to the left optic nerve, and 46.49 Gy to the optic chiasm. The tumor received a total radiation dose of 60 Gy from both initial and IMRT boost treatments in 30 fractions (see Figures 1 and 2).
Mr. L. had preexisting mild hypertension and was on irbesartan 150 mg daily. He had no preexisting or new-onset diabetes mellitus and no evidence of malignancy involvement in his optic nerves upon MRI. After losing his vision, Mr. L. had a flat affect and decreased interest in performing the activities of daily living. He developed depression but refused to take antidepressants. He suffered several falls in the home. Mr. L.’s son and grandson became actively involved in his care, which increased the family’s stress level. Mr. L. continued receiving bevacizumab therapy for a total of 2 years following his disease recurrence. Despite prolonged local disease control, Mr. L.’s quality of life decreased dramatically after he lost his ability to see.







