Abstract
Case Study
In early 2010, Mrs. Y., a 58-year-old Japanese woman, underwent a routine mammogram that revealed left focal asymmetry. A biopsy demonstrated invasive ductal carcinoma, and she was referred to surgery. She underwent a lumpectomy and left axilla sentinel lymph node biopsy. Pathology confirmed an invasive ductal adenocarcinoma, moderately differentiated, 1.2 cm, estrogen receptor (ER)/progesterone receptor (PR) negative, and HER2/neu negative with negative surgical margins. Three left axillary sentinel lymph nodes showed no evidence of disease.
Mrs. Y. was diagnosed with stage I T1cN0Mx breast cancer. Her oncologist estimated that she had a 25% 10-year risk of relapse and a 13% 10-year risk of mortality, with an estimated 35% mortality benefit conferred by adjuvant therapy. Although it was recognized that triple-negative breast cancer confers a worse prognosis (Foulkes, Smith, & Reis-Filho, 2010), no available prognostic calculators considered hormone receptor status; the oncologist’s projections were overly optimistic. In a recent retrospective study in triple-negative breast cancer patients, Hernandez-Aya et al. (2011) found a 5-year mortality rate of 16% for T1N0 patients and a 5-year relapse of 26% in these patients, similar to what Mrs. Y.’s oncologist had estimated for 10 years.
The oncologist recommended adjuvant therapy, and Mrs. Y. received four cycles of adjuvant docetaxel and cyclophosphamide followed by radiation therapy to the tumor bed and left breast. Her treatment followed the course recommended by the National Comprehensive Cancer Network Guidelines at that time (Carlson et al., 2009). She completed therapy in October 2010 without having experienced any dose reductions, delays, or complications.
Mrs. Y. continued to show no evidence of disease until early 2013, when she developed left neck and arm swelling. Computed tomography (CT) scan of the neck and thorax revealed a left supraclavicular mass compressing the left internal jugular and subclavian veins and enlarged cervical lymph nodes. A biopsy of the supraclavicular mass confirmed metastatic breast cancer. CT scan of the abdomen and pelvis showed no other sites of disease. She was treated with involved-field irradiation (16 Gy) to the sites of tumor recurrence and then was lost to follow-up.
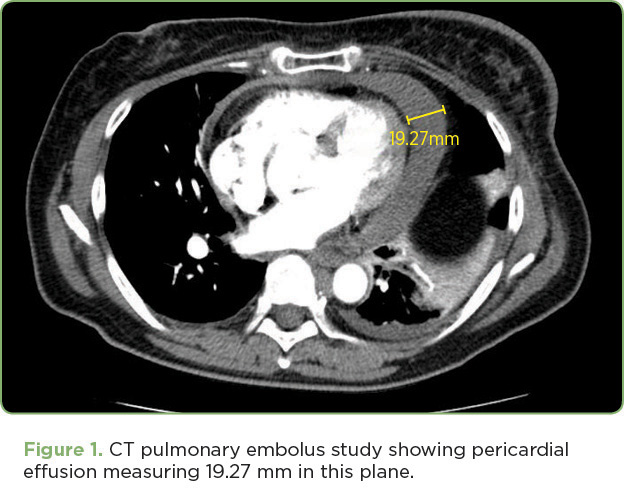
Six months following completion of irradiation, Mrs. Y. presented to the emergency department (ED) with dyspnea. On review of systems, she reported a 3-month history of a progressive cough and a 3-week history of hoarseness with progressive shortness of breath (SOB) and difficulty speaking. Upon physical examination, her voice was hoarse, breath sounds were clear to auscultation, and there were palpable left supraclavicular nodes. She did not have muffled heart sounds, elevated jugular venous pressure (JVP), or pulsus paradoxus. In the ED, her vital signs were blood pressure (BP) 129/85, pulse 89, oxygen saturation 98%, and respirations 16. An electrocardiogram (ECG) revealed sinus rhythm with borderline T-wave abnormalities in diffuse leads and a heart rate of 94. Her troponin I level was zero. A CT angiogram revealed a moderate-sized pericardial effusion (Figure 1) and supraclavicular and mediastinal lymphadenopathy with no evidence of a pulmonary embolus. Ultrasound confirmed a moderate pericardial effusion with no evidence of tamponade.
Overnight, Mrs. Y.’s SOB remained stable but her BP dropped to 70/49, which improved to 80/62 in response to a normal saline bolus. An ECG revealed sinus rhythm with partial resolution of the T-wave abnormalities and a heart rate of 65. Systolic blood pressure remained below 90 for several hours despite fluid boluses; by morning her BP had improved to 93/63. Echocardiography (echo) revealed a moderate-sized circumferential pericardial effusion with mild diastolic right atrium/right ventricle collapse, a dilated inferior vena cava, and mild mitral valve inflow variation with respiration, consistent with mild hemodynamic compromise. Left ventricle size and systolic function were normal.
Based on the echo findings, newly elevated JVP, and ongoing hypotension, Mrs. Y. was diagnosed with cardiac tamponade and suspected malignant pericardial effusion. Cardiology performed a diagnostic and therapeutic echo-guided pericardiocentesis and removed 260 mL of a bloody turbid fluid. A drain was left in, but it removed only 10 mL of fluid overnight and was removed the next day. Mrs. Y. had almost immediate relief of her dyspnea, and by day 3 she reported that she felt “a hundred times better” than she had at admission. She was discharged later that day after repeat echo showed a stable small pericardial effusion. Cytology of the pericardial fluid ultimately revealed metastatic adenocarcinoma consistent with the original breast cancer diagnosis.







