Abstract
Case Study
Mrs. K is a 63-year-old woman who presented to the clinic with complaints of fatigue, bruising, weight loss of 20 pounds in the past 2 months, and decreased appetite. She stated that she had constant moderately severe joint pain and napped three times a day in an attempt to battle her fatigue. However, the naps resulted in no change in her fatigue. Her increase in fatigue interfered with her daily functioning, and she was unable to enjoy spending time with her family.
Mrs. K's medical history included breast cancer diagnosed in 2006 and hypertension diagnosed in 2010. For her breast cancer, she was treated with chemotherapy and radiation therapy. She had no other pertinent medical history and no significant family history.
Physical examination revealed temperature of 38.9˚C, heart rate of 108 beats per minute, blood pressure of 158/68, respiratory rate of 22 breaths per minute, oxygen saturation of 96%; skin intact, pale, and cool to touch; scattered petechiae were present over both her lower extremities, abdomen, and back; and pale oral mucosa were observed. All other systems reviewed were unremarkable.
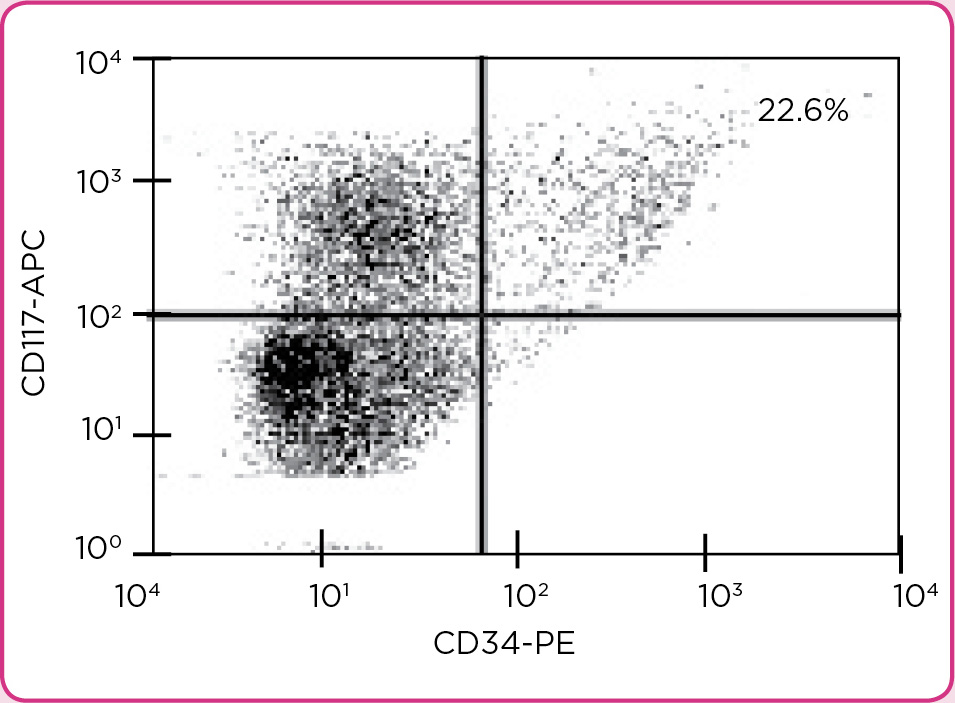
Laboratory workup revealed the following measures: peripheral blood with white blood cell count of 110,000 x 103/µL, hemoglobin of 8.6 g/dL, hematocrit of 28%, and a platelet count of 8,000 x 103/µL. A bone marrow biopsy evaluated by flow cytometry revealed 22.6% CD34+/CD117+ blasts (Figure 1).