Abstract
Case Study
Maria was a 23-year-old woman who initially presented with a 1-year history of pain in the left heel. Over time, the pain had progressively worsened. Eventually, her foot had swollen, and she had difficulty walking, which required her to seek medical attention.
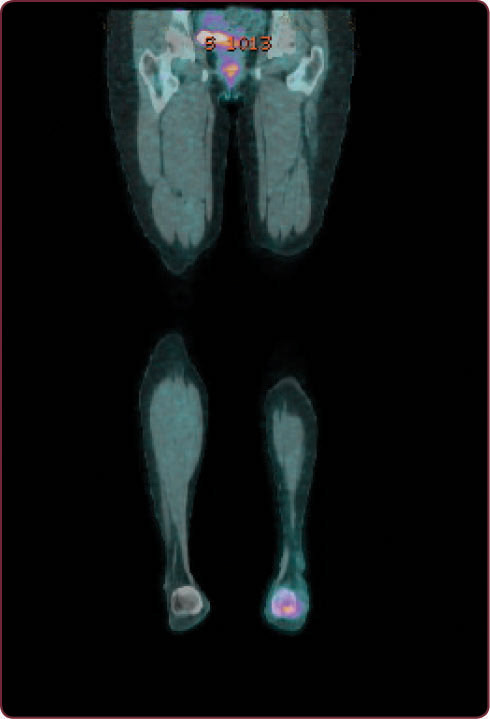
Initial imaging included a lower extremity magnetic resonance imaging (MRI) scan that revealed a malignant-appearing 5-cm lesion in the left calcaneus. A core needle biopsy showed bone that was infiltrated with poorly differentiated round malignant cells that were positive for CD99, which is consistent with a diagnosis of Ewing sarcoma. A staging positron-emission tomography–computed tomography (PET-CT) scan demonstrated a moderate hypermetabolic primary malignant lesion with a standardized uptake value (SUV) of 5.7 of the left calcaneus, as shown in the Figure below. The result also showed multiple mild hot spots in the bony skeleton, including the lumbar spine at L3 and L5 vertebral bodies, the right femur, and the left femur, suspicious for metastatic disease. In addition, the PET-CT showed numerous small lung nodules that were too small to characterize. Maria denied a fever or weight loss but did complain of fatigue. Her laboratory values were within normal limits.
At our hospital’s sarcoma tumor board meeting, a multidisciplinary team discussed the treatment plan for all patients with sarcoma. For Maria, we decided that based on her PET-CT scan, she had metastatic disease. We agreed it was best to treat her systemically with combination chemotherapy. In preparation of anthracycline chemotherapy, a two-dimensional echocardiogram was completed, and it showed an ejection fraction of 60%. We also discussed fertility preservation with Maria and her husband. They chose not to have egg preservation, but she started on monthly leuprolide injections. She was admitted to the inpatient oncology unit to begin chemotherapy, which included cyclophosphamide, doxorubicin, and vincristine with alternating cycles of ifosfamide and etoposide.







