Abstract
Case Study
Tom, a 75-year-old white male, was recently diagnosed with metastatic renal cell carcinoma (RCC; Tom’s case is not an actual clinical case but has been developed by the authors as an exemplar). Two years prior, he had undergone a left partial (laparoscopic) nephrectomy for clear cell RCC. At that time, he had a stage 3 disease (the tumor extended into perinephric tissues but not into the ipsilateral adrenal gland and not beyond Gerota’s fascia [Cancer.net, 2016]), and regularly (every 3–6 months) scheduled surveillance imaging did not show metastatic disease. Recent imaging with a computed tomography (CT) of the chest/abdomen/pelvis revealed small bilateral pulmonary nodules that did not have the radiographic appearance of a primary lung tumor, but rather that of metastatic disease. Therefore, a decision was made to repeat CT scans in a shorter interval (in 6 weeks) to assess growth kinetics. Subsequent CT scan showed an increase in size and number of pulmonary nodules, so the decision was made to begin systemic treatment.
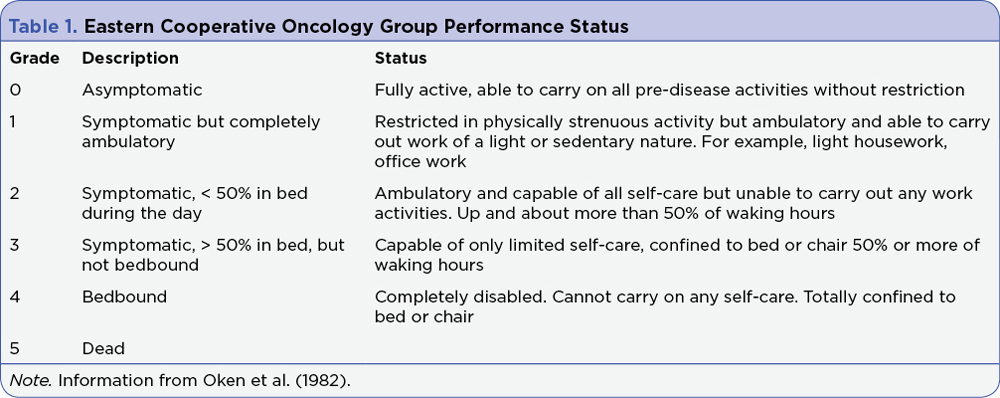
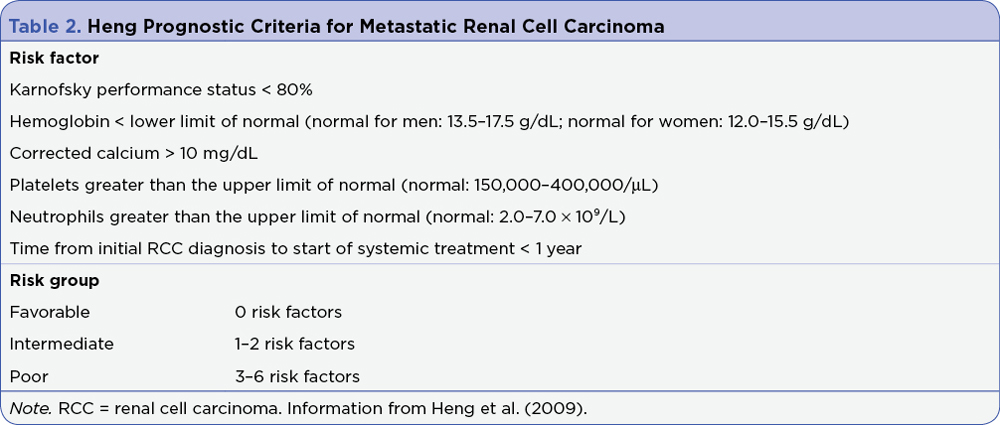
At the time of Tom’s metastatic evaluation, his Eastern Cooperative Oncology Group performance status was 0 as he was asymptomatic and fully active (Table 1). He was classified as favorable risk according to Heng criteria (Table 2). Tom is married and lives with his wife. He is independent in his self-care but also relies on his wife for health-care decision-making. He does not drink alcohol and is a former smoker with a history of 30 pack-years. Tom’s medical history includes hypertension that is adequately controlled with lisinopril (20 mg/day), coronary artery disease (on daily aspirin 81 mg) with left ventricular ejection fraction (LVEF) of > 50%, which is within the normal range (50%–75%), benign prostatic hyperplasia for which he is treated with finasteride, and hyperlipidemia that is treated with atorvastatin.